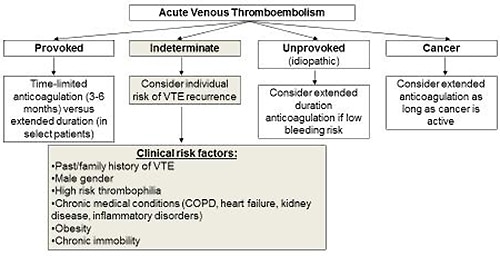
Determining the optimal duration of anticoagulation after deep vein thrombosis or PE requires an individualized assessment of the patient’s preferences as well as long-term risk of recurrence and bleeding (Figure 2). A number of strategies can be utilized to help the physician make this decision. The 2016 American College of Chest Physician guidelines recommend anticoagulation of three months for provoked VTE and extended duration for patients with a low to intermediate bleeding risk and unprovoked (idiopathic) VTE . Other approaches involve assessment of each individual’s clinical risk factors for recurrence and laboratory testing for hypercoagulability, or post-treatment D-dimer levels.
Patients with VTE and cancer have an increased risk of recurrence and are generally prescribed extended duration anticoagulation with LMWH as long as they have active malignancy. Similarly, VTE patients with severe thrombophilia, such as those with the antiphospholipid syndrome (positive lupus anticoagulant, anticardiolipin antibodies, anti-prothrombin antibodies, and anti-β2 glycoprotein-1 antibodies) or deficiencies of protein C, S, or antithrombin are often prescribed extended duration anticoagulation because of a high risk of recurrence. Although not endorsed by published evidence-based guidelines, a patient-specific strategy utilizing D-dimer testing and/or lower extremity venous imaging after completion of standard anticoagulation for VTE has been evaluated to determine the optimal duration of anticoagulation. However, a clinical study by Kearon C and colleagues found that the risk for recurrence in patients with a first unprovoked VTE who had a negative D-dimer results was not low enough to justify stopping anticoagulation. Other chronic medical conditions that predispose to VTE, such as chronic obstructive pulmonary disease, heart failure, systemic inflammatory disorders, and obesity, may also be considered in the decision-making regarding length of therapy.