Once the diagnosis of PE is suspected, anticoagulation should be started immediately unless there is a contraindication such as active or a high risk of bleeding, which should be assessed in all patients before and during anticoagulation therapy. In addition to anticoagulants, other more aggressive therapies such as systemic thrombolysis or catheter-directed thrombolytic or pharmaco-mechanical therapies, surgical intervention (acute pulmonary embolectomy) or placement of an inferior vena cava (IVC) filter may be appropriate.
Anticoagulants are used in the acute (first 0 to 7 days), long-term (7 days to 3 months), and extended (3 or 6 months to indefinite) treatment phases of PE. For more details please see (Table 4)
Table 4: Anticoagulation Used in Acute, Long-term and Extended Treatment Phases (three month to indefinite).
| Anticoagulants |
Acute phase (0-7 days) |
Long-term phase (7 days – 3 months) |
Extended phase + (3 or 6 months to indefinite) |
| Apixaban |
Apixaban 10 mg twice daily X 7 days |
Apixaban 5 mg twice daily times 3 months |
Apixaban 2.5 mg twice daily |
| Rivaroxaban |
Rivaroxaban 15 mg twice daily X 21 days |
Rivaroxaban 20 mg daily times 3 months |
Rivaroxaban 10 mg daily |
| Dabigatran* |
Heparin, low molecular weight heparin or fondaparinux |
Dabigatran 150 mg twice daily times 3 months |
Dabigatran 150 mg twice daily |
| Edoxaban* |
Heparin, low molecular weight heparin or fondaparinux |
Edoxaban 60 mg daily
Reduce edoxaban dose to 30 mg daily if CrCl is 15 to 50 ml/min or weight ≤60 kg or use of strong P-gp inhibitor |
|
| Warfarin * |
Heparin or low molecular weight heparin or fondaparinux |
Warfarin dosing with INR goal of 2-3 |
Warfarin dosing with INR goal of 2-3 |
| Low molecular weight heparin (Enoxaparin) |
*Low molecular weight heparin at dose of 1 mg/kg every 12 hours x 5-10 days as initial treatment for patients receiving dabigatran, edoxaban or warfarin |
Low molecular weight heparin at dose of 1 mg/kg every 12 hours or 1.5 mg/ kg daily for cancer or pregnant patients |
Low molecular weight heparin at dose of 1 mg/kg every 12 hours or 1.5 mg/ kg daily for cancer or pregnant patients |
| Fondaparinux |
*Fondaparinux at 5 mg for patients less than 50 kg, 7.5 mg for patients >50 kg to <100 kg and 10 mgs for patients >100 kg x 5-10 days as initial treatment for patients receiving dabigatran, edoxaban or warfarin |
|
|
| Heparin |
*80 units/kg bolus followed by 18 units/kg continuous infusion x 5-10 days as initial treatment for patients receiving dabigatran, edoxaban or warfarin |
|
|
*Indicates anticoagulants that require 5 to 10 days of a parenteral overlap
Clinical trials evaluating efficacy of apixaban 2.5 mg and rivaroxaban 10 mg started patients on these doses after 6 months of initial anticoagulant therapy with doses of apixaban 5 mg twice a day and rivaroxaban 20 mg daily respectively.
Dosing recommendations may vary depending on age, renal function, and body weight. These are general recommended doses for most patients however providers should always consult the package insert or other dosing resource when prescribing for elderly, those with renal dysfunction, or extremes of weight.
The choice of anticoagulants depends on the clinical indication and the patients underlying condition, patient’s preference and risk of bleeding. Heparin, the low molecular weight heparins (LMWHs), fondaparinux or the direct oral anticoagulants (DOACs) including rivaroxaban and apixaban are the only agent’s recommended (FDA approval) for acute phase treatment while warfarin and the DOACs (rivaroxaban, apixaban, dabigatran and edoxaban) are options for long-term anticoagulation. The LMWHs should be used for the patient with cancer and during pregnancy.
Outpatient Therapy or Early Discharge of Pulmonary Embolism
The majority (>90%) of patients diagnosed with PE are hospitalized for treatment even if the primary therapy is anticoagulation alone. The most common reason for hospitalization is fear of adverse events such as hemodynamic decompensation, recurrent or worsening thromboembolism and major bleeding any of which could lead to increased morbidity and mortality. Recent randomized controlled trials have demonstrated that the risk of death from either PE or major bleeding after an acute event is <0.5%. Additionally venous thromboembolism (VTE) recurrence was only found in 3.7 and 4.1 per 100 patient-years and major bleeding was only 1.8 and 3.1 per 100 patient-years in patients on direct oral anticoagulants and vitamin K antagonist respectively.
There are several benefits of outpatient therapy for PE such as better quality of life, patient satisfaction, as well as early return to work and other professional and personal activities. It also reduces or eliminates hospital acquired complications including infection. Outpatient PE therapy may also reduce treatment costs and overcrowding in the hospital.
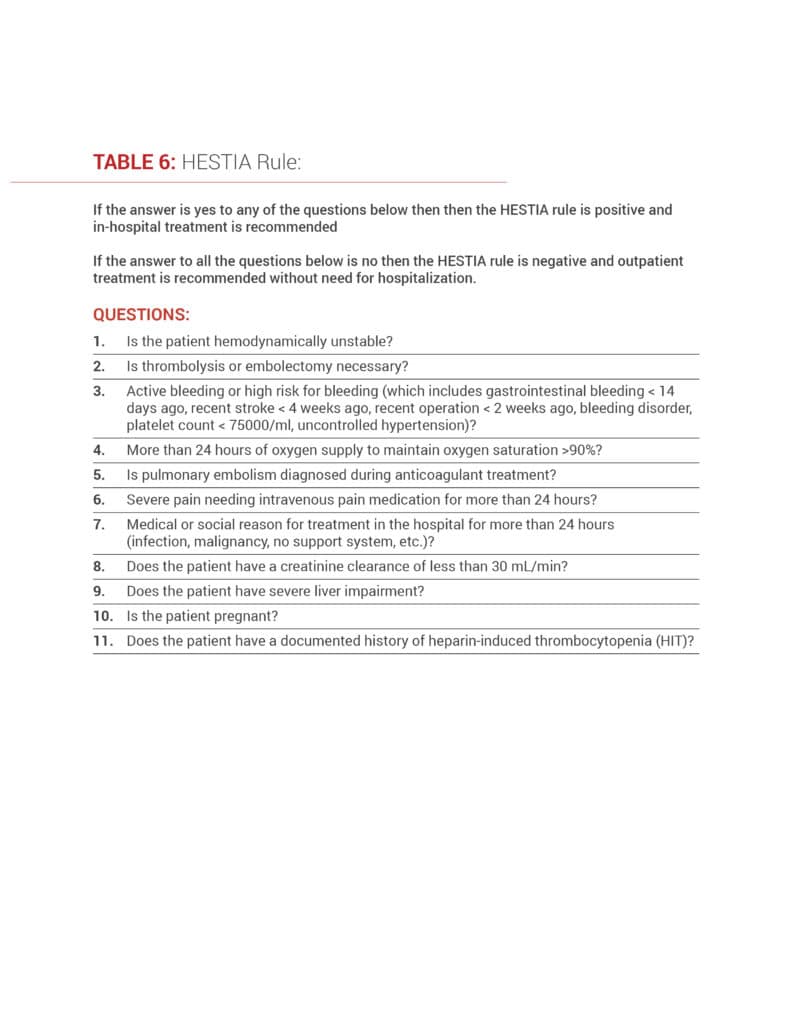
Recently, there have been a number of clinical studies performed to define the subset of patients with PE at low risk for early mortality and adverse outcomes in order to systematically identify those individuals who can be treated as an outpatient or discharged early from the emergency room or after a short-stay hospitalization. A meta-analysis of patients with acute PE managed at home or early discharge from the hospital using the original Pulmonary Embolism Severity Index (PESI) that looked at 11 factors, simplified PESI (sPESI) 6 factors, or HESTIA rule (11 factors) (see tables below) developed criteria for this purpose. Using these criteria, early complication rates (1-3 months) including thromboembolic recurrences or major bleeding was <2% and early mortality (30-day) was < 3%.
Current clinical guidelines from the American College of Chest Physicians and the European Society of Cardiology suggest outpatient management or early discharge for patients with low PESI scores Class I or II, (Table 5) and if home circumstances are appropriate and proper outpatient care can be provided.
The HESTIA rule is another approach to determining if the patient is a good candidate for outpatient therapy (Table 6).
Studies have shown that a low simplified PESI score (<1) is similar to a low original PESI score (class I and II) in identifying patients at low risk for short-term mortality from PE. Using the simplified PESI score may be more time-efficient and less cumbersome since only 6 factors are assessed. The presence of any of these factors automatically rules out patients for consideration of outpatient therapy. In contrast, the original PESI risk calculator uses 11 factors with different points for each factor and requires more calculation and time to identify the low risk patient. We recommend using PESI, simplified PESI or HESTIA rule for assessing patients.